Over the last few weeks, I’ve noticed the resurgence of messaging that emphasizes “natural immunity” as being superior to vaccine-induced immunity to COVID-19, particularly for the more recent variants of SARS-CoV-2, such as Delta, Omicron, and, most recently, the Omicron subvariant BA.2. For example, Jeffrey Tucker published an article at the Brownstone Institute website asking “Are They Finally Admitting Natural Immunity?”, as though public health officials have somehow been “covering up” this “natural immunity”, the better to keep enforcing “lockdowns” and masking and vaccine mandates. (Translation: “Natural immunity” is the way out of the pandemic that “they” don’t want you to know about.) Meanwhile, conservative-leaning mainstream media outlets like Fox News and The Wall Street Journal have had a number of stories and articles touting “natural immunity”, with, as just one of many examples, Johns Hopkins surgical oncologist Dr. Marty Makary having tried to portray a “high cost of disparaging natural immunity to COVID-19” and claiming that public health officials have “ruined many lives by insisting that workers with natural immunity to Covid-19 be fired if they weren’t fully vaccinated”. This narrative has, in particular, been deployed to defend the Canadian trucker convoys that recently besieged Ottawa and, just across the river from me in Windsor, blocked the Ambassador Bridge to Detroit in order to protest Canadian vaccine mandates.
Before I get to the science, in the interests of transparency I like to make my position clear. The term “natural immunity” is a very poor descriptor whose very use of the word “natural” has made it very easy for ideologues and antivaxxers to weaponize to argue against COVID-19 vaccines and restrictions. I’ve discussed before, as has Alan Levinovitz, how scientists made a huge mistake in adopting the term “natural immunity”. The reason is that it is an inherently misleading term; people often view naturalness as synonymous with purity and goodness. Moreover, vaccine-induced immunity is every bit as “natural” as post-infection immunity (the more appropriate term to describe immunity after an infection), with the added huge advantage of not having to suffer through the disease and risk its potential complications, up to and including death, to acquire immunity. Worse, advocates of “natural immunity” not limited to antivaxxers frequently describe this immunity as having quasi-magical properties, implying that it is lifelong, far better against everything, and even beneficial, with some even going so far to argue that it’s better, for instance, to let children become infected. (Of course, even though children do have a much lower risk of severe disease and death from COVID-19, there are those pesky large—for children—COVID-19 death tolls that rebuke this argument every bit as much as the death toll in the US that is now approaching one million rebukes previous predictions that we would achieve herd immunity soon.)
Sadly, it’s not just antivaxxers and antimaskers who have started promoting the “natural immunity” narrative in which letting COVID-19 rip through the “healthy” population and children will get us to “natural herd immunity” faster than just vaccination campaigns. It’s doctors who should know better. As a result, increasingly activists, pundits, and politicians—sadly, including some doctors and scientists—opposed to vaccine and COVID-19 mandates of any kind are co-opting the term “natural immunity” to give anyone previously infected and recovered a free pass from any restrictions, sometimes taking the idea to ridiculous extremes.
Leaving aside my contention that “natural immunity” is a horrible term (which is why I never use it except with scare quotes), what is the real situation? As is often the case with such issues, it’s complicated. We cannot discuss this question, however, without taking a look at the dominant narrative with respect to “natural immunity”, in particular because the science is not consistent with this narrative.
The Great Barrington Declaration
I debated about whether to bring up the Great Barrington Declaration (GBD) yet again, having done so just last week in the context of John Ioannidis’ awful “study” that attempted to argue that the GBD was somehow overwhelmed in the social media narrative by “science Kardashians” with far more Twitter firepower than scientific contributions. It is an article that is being used by GBD advocates to cast opponents as unserious social media creatures. However, it is appropriate, given how the GBD, its authors, its signatories, and its boosters have dominated the media narrative on “natural immunity” and “natural herd immunity”.
The ideas behind the GBD, which was first published in October 2020 (before safe and effective COVID-19 vaccines were available to the public anywhere except in clinical trials) were threefold. First, “lockdowns” (however you define “lockdown”, and GBD proponents seem to define it as any government public health edict closing or restricting businesses or placing any restrictions whatsoever on private individuals) do far more harm than good. Second, “natural herd immunity” is inevitable, and, therefore third, we should adopt a “let ‘er rip” strategy with respect to COVID-19 and the “healthy” and “young” population and use “focused protection” to keep those at high risk of serious disease, complications, and death from COVID-19, safe. Moreover, contrary to their penchant for describing themselves as “silenced“, GBD authors and advocates have long had preferential access to media and government officials. Indeed, as Stanford PhD student Mallory Harris has noted, the recent release of a book by Scott Atlas, President Trump’s COVID-19 advisor, basically confirmed this preferential access:
Problems abounded with the GBD with respect to all three ideas behind it. First, its adherents tended to vastly exaggerate the harms of “lockdowns” and minimize the ability of “lockdowns” and other mandates, such as masks (collectively known as nonpharmacological interventions, or NPIs), to slow the spread of COVID-19, an issue still debated today, while promoting a caricature of public health officials as completely ignoring any negative consequences of such policies in relation to potential benefits.
Second, the assumption that “natural herd immunity” was inevitable was just that, an assumption. “Natural herd immunity” is the epidemiological principle that over time an infectious disease will infect enough of the population to produce enough post-infection immunity to result in herd immunity, the level of immunity at which the number of new infections reaches a steady state and there are no longer large spikes in incidence and epidemics. Because such immunity required that a huge fraction of the population suffer through the disease, GBD adherents had to bend over backwards to portray COVID-19 as a “mild disease” by lowballing death estimates and portraying it as “harmless” to children. More importantly, “natural herd immunity” also requires that post-infection immunity be long-lived, if not life-long. If immunity wanes too quickly in individuals or virus variants crop up that can evade the immunity from previous infections, “natural herd immunity” will likely never be reached. I can only cite Omicron and the new Omicron subvariant BA.2 as evidence that this has been the case with COVID-19, but even 16 months ago given how the Omicron variant has led to a massive surge in reinfections, despite all we didn’t know, we did know that post-infection immunity to coronaviruses is often transient and that variants that evade immunity commonly develop. Even as long as a year ago, scientists were beginning to fear that herd immunity even as a result of post-infection immunity plus vaccine-induced immunity was probably out of reach because too high a percentage of the population would need to be immune, waning immunity (both vaccine- and infection-induced), insufficient prevention of forward transmission of the virus, and new virus variants, all the failed predictions of academics like Dr. Makary about how soon we will have “herd immunity” notwithstanding.
Finally, the concept of “focused protection” in the GBD was ill-defined to the point of being basically meaningless (and remains so today). It ignored the incredible difficulty—if not impossibility—of protecting the large segment of the population that is at high risk of severe disease and death, including the elderly and those with chronic health conditions, while a respiratory virus is ripping through the young, “healthy” population, while seemingly arguing just keeping the elderly and high-risk population locked away from society indefinitely to “protect” them while not unduly inconveniencing everyone else. It was a profoundly ableist and, dare I say, even eugenicist idea couched in terms of claiming that letting the young be infected would somehow also protect the vulnerable. It was always nonsense, a politically motivated faux proposal given that it originated in a conference organized by a right wing think tank opposed to “lockdowns” and other COVID-19 restrictions.
The political use and misuse of “natural immunity,” particularly by GBD-linked sources like the Brownstone Institute notwithstanding, it is worth reviewing recent evidence to evaluate the relative value of post-infection immunity. It’s also worth doing so in the context of the narrative of GBD-linked sources, such as the Brownstone Institute, whose founder recently asked the question about “admitting” to “natural immunity”. Why? Because Tucker references a recent CDC study to make his claim:
In late January, the CDC published a report that made what might have been regarded as a shocking claim. If you have had Covid, the CDC demonstrated in a chart, you gain robust immunity that is better than that of vaccination, especially concerning duration.
That should be nothing surprising. Brownstone has chronicled 150 studies making that point. What made this new chart different was that it came from the CDC, which has buried the point so deeply for so long as to amount to a near denial.
So there: the CDC says it. So nonchalant! So uneventful!
If people had understood this two years ago, plus been made more completely aware of the dramatic risk gradient by age and health, lockdowns would have been completely untenable.
The society-wide mandates and lockdowns depended on keeping the public ignorant on settled points of cell biology and immunology, plus pressuring social media companies to censor anyone who didn’t fall in line. Here we are all this time later and the truth is coming out.
Had the knowledge of risk gradients and immunities been in the forefront of policy makers’ minds – instead of wild fear and obsequious deference to Fauci – we would have focused on protecting the vulnerable and otherwise allowed society to function normally so that the virus would become endemic. We would not only have saved thousands of lives; we could have avoided the vast economic, educational, cultural, and public-health wreckage all around us.
Those poor, “silenced” advocates for “natural herd immunity”! Note the way that Brownstone writer Paul Alexander—yes, that Paul Alexander, the HHS science advisor who once wrote in an email that we “want them [infants, kids, teens, young people, young adults, middle aged with no conditions] infected” to reach “natural herd immunity”—conflates number of studies with quality of data – a favorite tactic among antivaxxers as well. Note also how he blamed Anthony Fauci for it all, even though many months went by in 2020 when Trump barely spoke to Fauci because he didn’t like what Fauci had to say.
But what about that study? The narrative lately appears to be a tale of a couple of recent studies, which starts with the CDC study.
Did the CDC really say that “natural immunity” to COVID-19 is superior?
The study referenced by Tucker was published three weeks ago in Morbidity and Mortality Weekly Report (MMWR), the chief scientific outlet of the CDC, and he is quite taken by a video “analysis” written by Dr. Vinay Prasad. Before the pandemic, Dr. Prasad was known for critiquing the sometimes poor quality of clinical evidence used in oncology and other medical specialties, although even before the pandemic he had little but contempt for those of us who take the time to refute quackery and antivaccine misinformation. It’s ironic, then, how since the pandemic he’s pivoted to becoming a rich (and, to the public, an unfortunately seemingly authoritative) source of such misinformation, even describing public health interventions as potentially the first step on the road to fascism.
His entire claim is based on this graph from the paper:
This graph does a lot of work in “natural immunity” land.
This figure represents data from California and New York (which account for 18% of the U.S. population) in order to assess what happened as the Delta wave became predominant, with the CDC stating in the discussion:
Across the entire study period, persons with vaccine- and infection-derived immunity had much lower rates of hospitalization compared with those in unvaccinated persons. These results suggest that vaccination protects against COVID-19 and related hospitalization and that surviving a previous infection protects against a reinfection. Importantly, infection-derived protection was greater after the highly transmissible Delta variant became predominant, coinciding with early declining of vaccine-induced immunity in many persons (5). Similar data accounting for booster doses and as new variants, including Omicron, circulate will need to be assessed.
So what we have is a snapshot of what happened as the Delta wave ramped up but before Omicron crashed onto the scene, which led to different results than what were observed with the original COVID-19 strain, for which vaccine-induced immunity was more potent than post-infection immunity. Is this slam-dunk evidence that “natural immunity” is superior? Not exactly. As the CDC notes, these data don’t come close to taking into account the Omicron variant and the effect of the increasing number of people receiving boosters. Indeed, the CDC noted at least seven limitations, among them no stratification of the analysis by time since vaccine receipt; misclassification of persons with undiagnosed COVID-19 infection as having had COVID-19, which would decrease apparent differences between the vaccinated and unvaccinated; unmeasured confounding due to differential risk; no information on severity of initial infection; lack of ascertainment of receipt of additional or booster COVID-19 vaccine doses, given that the study was conducted before many persons were eligible or had received additional or booster vaccine doses; lack of precision in some samples due to sample size limitations; and the fact that the analysis was carried out before Omicron.
Indeed, another analysis that tries to do that (referenced in the article) is not nearly as clear:
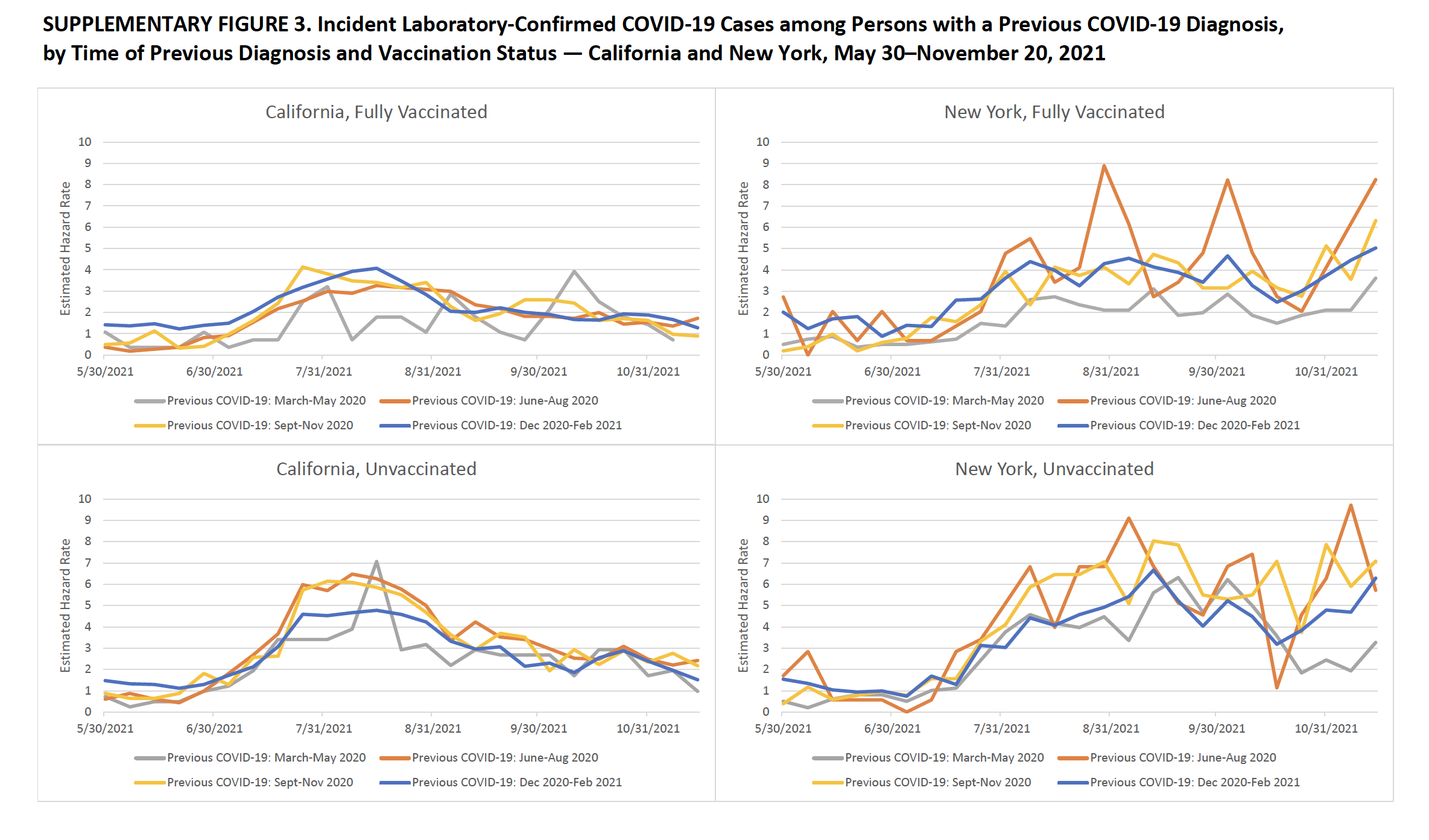
The data don’t look quite as clean when presented this way.
That’s why the CDC concluded:
Vaccination protected against COVID-19 and related hospitalization, and surviving a previous infection protected against a reinfection and related hospitalization during periods of predominantly Alpha and Delta variant transmission, before the emergence of Omicron; evidence suggests decreased protection from both vaccine- and infection-induced immunity against Omicron infections, although additional protection with widespread receipt of booster COVID-19 vaccine doses is expected. Initial infection among unvaccinated persons increases risk for serious illness, hospitalization, long-term sequelae, and death; by November 30, 2021, approximately 130,781 residents of California and New York had died from COVID-19. Thus, vaccination remains the safest and primary strategy to prevent SARS-CoV-2 infections, associated complications, and onward transmission. Primary COVID-19 vaccination, additional doses, and booster doses are recommended by CDC’s Advisory Committee on Immunization Practices to ensure that all eligible persons are up to date with COVID-19 vaccination, which provides the most robust protection against initial infection, severe illness, hospitalization, long-term sequelae, and death.
So, basically, yes, in this one study looking at the original COVID-19 strain and the Delta variant, post-infection immunity appears to be more robust, but with a lot of caveats, none of which stopped GBD adherents from claiming that this study was slam dunk evidence that “natural immunity” is “6x better than vaxx.” Again, let’s just say that it’s way more complicated and nowhere near that clear, even if you look at just this CDC study.
The “natural immunity” wars continue
There are, of course, a number of other studies, and, taken together, what they say about post-infection versus post-vaccination immunity is…confusing, at best. For example, here’s one study, published in JAMA, that GBD proponents were touting last month. It’s from Dr. Makary’s group, which isn’t a good sign, and it examined only antibody levels. Worse, get a load of its recruitment methods:
Healthy adults who reported no SARS-CoV-2 vaccination were recruited via 1 public Twitter post and 1 public Facebook advertisement between September 11, 2021, and October 8, 2021. Participants completed an online questionnaire about demographics, COVID-19 status, and mask use. Using weighted random sampling (relative weights based on the estimated unvaccinated US population by age, race and ethnicity, and education1), we created 3 equally sized sample groups among those who reported a test-confirmed COVID-19 infection (“COVID-confirmed”), believed they had COVID-19 but were never tested (“COVID-unconfirmed”), and did not believe they ever had COVID-19 and never tested positive (“no-COVID”). These groups were invited to undergo antibody testing at LabCorp facilities nationwide.
Yes, you read that right. There’s no control group, and recruitment was by a highly dubious method. Yet Makary misrepresented his paper on Twitter thusly:
Our Natural Immunity Study out today in JAMA:
👍🏼816 people
👍🏼99.3% with prior Covid had circulating antibodies (unvax)
👍🏼Durable for ~2yrs studied
👍🏼Lexicon of immune/non-imm >> vax/unvax
👍🏼Don't try to get Cov. But if you had it, imm more durable than vax https://t.co/mlR2GIhzOh https://t.co/PuP1L1cNIi pic.twitter.com/7tLqPlbIvk— Marty Makary MD, MPH (@MartyMakary) February 3, 2022
I am simply going to go right to the Discussion section to quote Dr. Makary and colleagues themselves:
Study limitations include lack of direct neutralization assays, the fact that antibody levels alone do not directly equate to immunity,4,6 the cross-sectional study design, a convenience sample with an unknown degree of selection bias due to public recruitment, self-reported COVID-19 test results, the study population being largely White and healthy, and lack of information on breakthrough infections. Participants were given only 1 month to complete antibody testing, which may have contributed to the 52% rate among those invited to test.
Plus this rather…harsh…takedown that is, in my opinion, entirely justified:
9/U
And no, I'm not cherry-picking when I focus on neutralization.
For example, neutralization is central for assessing topics Makary has fabricated about for awhile now, such as herd immunity and viral transmission.https://t.co/nsphk6rXlThttps://t.co/bNMPMfg1pj pic.twitter.com/Vx1QXUUocD
— Atomsk's Sanakan (@AtomsksSanakan) February 10, 2022
11/U
Here's the thing, though:
Anybody reading the literature knew that already for months. 🤷♂️https://t.co/nAhAMTyEbvhttps://t.co/omBjxPdkov
[https://t.co/vTxjjftrIu]https://t.co/5wXXCMXkPMhttps://t.co/2cSjh5qgMEhttps://t.co/gSdvM0uEiyhttps://t.co/T5reK822yI pic.twitter.com/PM5Ok1KHR4— Atomsk's Sanakan (@AtomsksSanakan) February 10, 2022
Another study was published as correspondence to the New England Journal of Medicine from Qatar suggested that previous infection also protected against the Beta variant (B.1.3510), just not as much as against the original Alpha variant up to a year later, while earlier data from Qatar found that those who were reinfected were 90% less likely to be hospitalized or to die. Still more recent data from Qatar find that infection with a previous variant is only 56% protective against Omicron.
Then there is another recent Nature paper that used both antibody quantification and functional neutralization assays for antibodies against the SARS-CoV-2 spike protein receptor binding domain (RBD), which is responsible for binding to the ACE2 receptor on cells in order to facilitate the entry of the virus into the cell to do its dirty work, to assess the immune responses in convalescent plasma after infection compared to plasma from vaccinated individuals against various SARS-CoV-2 variants. To boil it down:
In this study, we showed that mRNA vaccinated blood donors have a median of 17 times higher RBD antibody levels when compared with those who became seropositive due to prior COVID-19. Our results indicated an exceptional strong association between high RBD antibody levels in and the ability to biochemically neutralize RBD binding to the cellular ACE2 receptor. The N501Y mutation, while did not alter the neutralizing antibody binding, presented with a fivefold greater affinity to ACE2, which resulted in a drastically reduced ability of COVID-19 convalescent antisera to neutralize its ACE2 binding. Fortunately, the vaccinated blood samples, due to their much-elevated RBD antibody levels, were far more effective in neutralizing both the WT and N501Y RBD from binding to ACE. With an average of 16-fold greater potency than convalescent blood, the vaccinated blood samples were more than sufficient to compensate for the fivefold increased affinity of N501Y RBD, resulting in the highly effective inhibition of both the WT and N501Y RBD from binding to ACE2.
That last part is important. The mutation that results in Omicron’s immune escape doesn’t so much decrease antibody binding to RBD as it results in an RBD that is a lot “stickier” to the ACE2 receptor, which means that it’s more likely to bind to the ACE2 receptor before an antibody can bind to it and neutralize it than is the case for the RBD of previous variants of SARS-CoV-2. Again, this study is preliminary, involving only 33 donors with previous COVID-19 plus 38 samples obtained from the Department of Laboratory Medicine of NIH as diagnostics samples and 28 people who received mRNA vaccines against COVID-19. Moreover, this study also suggests waning antibody levels after vaccination at 6 months, consistent with recent prior studies.
From my perspective, boiling it all down from the studies above and the ones cited in the above Twitter discussion, for now it does appear that infection-induced immunity is roughly as efficacious as the mRNA vaccines, not including boosters, and, like the vaccines, not as effective against later variants, an entirely expected finding that just needs quantification of how much less effective “natural immunity” is against later variants. Regardless of whether one views this “natural immunity” as superior or more robust than immunity from the vaccines, contrary to the claims made by boosters—if you’ll excuse the term—of “natural immunity” and “natural herd immunity,” even by the most optimistic metrics post-infection immunity is nowhere near lifelong and probably doesn’t last a lot longer than post-vaccination immunity, particularly for new variants. Indeed, even if post-infection immunity were to be found to persist two or three times longer than post-vaccination immunity, that would still be nowhere near good enough to make “natural herd immunity” a viable strategy to end the pandemic, particularly with the emergence of new variants and the variability in immune response after infection.
Again, it’s simplistic to look only at the “natural”/vaccine-induced immunity dichotomy, which brings me to “super” immunity and hybrid immunity. A better question is: How do we optimize protection against COVID-19, regardless of prior infection status and variant?
“Super-immunity” (a.k.a. hybrid immunity)
There are now a number of studies looking at what is known as “hybrid immunity,” or immunity to COVID-19 produced as a result of the combination of infection and vaccination, whether it’s as a result of a “breakthrough” infection after vaccination or of vaccination after a previous COVID-19 infection. Unfortunately, there’s another term that is being used for this type of immunity:
Another study, conducted by Oregon Health & Science University, found that a breakthrough infection in a vaccinated person leads to “super immunity.” The study compared blood samples from 52 Pfizer-vaccinated employees of the university infected with different strains of the virus—Alpha, Beta, Gamma, and Delta.
The study found that antibodies measured after breakthrough cases were more abundant and more effective than antibodies generated two weeks after a second dose of the Pfizer vaccine. “You can’t get a better immune response than this,” said Fikadu Tafesse, the author of the report and an assistant professor at the OHSU School of Medicine.
Regular readers likely could easily have predicted that I would absolutely detest the term “super immunity,” even more than I detest the term “natural immunity.” I realize that it’s probably an attempt from public health officials and scientists to counter the term “natural immunity,” but, if anything, “super immunity” is more misleading than “natural immunity,” which is why I prefer the more neutral term “hybrid immunity.” But what about that study and a number of others either published or in the pipeline of pre-prints? It’s possible that I might have missed a study, but let’s look at a quick rundown of what I did find.
There is a recent Israeli study published in Annals of Internal Medicine that’s a retrospective cohort that compared incidence rate of SARS-CoV-2 reinfection in previously infected persons to that of previously infected persons who subsequently received a single dose of the Pfizer-BioNTech mRNA vaccine using the centralized database of Maccabi Healthcare Services in Israel. This study has the drawback that the data used were largely from before the rise of the Omicron variant; and so nothing about non-Delta variants could be inferred. Nonetheless:
A statistically significant decreased risk (hazard ratio, 0.18 [95% CI, 0.15 to 0.20]) for reinfection was found among persons who were previously infected and then vaccinated versus those who were previously infected but remained unvaccinated. In addition, there was a decreased risk for symptomatic disease (hazard ratio, 0.24 [CI, 0.20 to 0.29]) among previously infected and vaccinated persons compared with those who were not vaccinated after infection. No COVID-19–related mortality cases were found.
There was no statistically significant difference in hospitalizations, though, likely because only 10 patients were hospitalized. That’s why a certain doctor whom we’ve met before and who should know better is claiming that this study shows no additional benefit from vaccination after infection, while labeling it the “best” study (because, of course, any study that reinforces your prior beliefs is the “best”). Let’s just say that it’s not the best (although it is good), but the point is taken that, in this study, both groups did so well that the numbers of hospitalized patients were too small to determine if there was a statistically significant difference between them, while the hazard ratios for infection and statistical disease revealed an impressive decline in the risk of Delta in those recovered from prior infection who received a dose of the Pfizer vaccine that would lead me to predict that a larger study would have found differences in hospitalizations, too.
More interestingly, there were two studies published in last week’s NEJM addressing this question as well, one from the SIREN (SARS-CoV-2 Immunity and Reinfection Evaluation) study group and another from an Israeli group. The SIREN study is a multicenter, prospective cohort study involving health care workers in the United Kingdom and consisting of asymptomatic adults who underwent polymerase-chain-reaction (PCR) testing every 2 weeks, among whom more than 30% of the participants were seropositive for SARS-CoV-2 at enrollment. The Israeli study is another retrospective cohort study using two databases maintained by Clalit Health Services. Both suggest the same thing, that hybrid immunity is superior to either post-vaccination or post-infection.
The SIREN study was begun in June 2020 and for this NEJM publication included 35,768 participants, of which 27% (9,488) had a previous SARS-CoV-2 infection. Because of the prospective nature of the study, it was possible to follow these participants over time and determine infection and reinfection risk for various cohorts. The study found that, although the Pfizer/BioNTech vaccine provided excellent short term immunity, its immunity waned after 6 months, while immunity from prior infection was waning after a year. The very best immunity came from a combination of prior infection and vaccination, which remained robust after a year.
The second study, from Israel, also found that the cumulative risk of reinfection was much lower in those who were vaccinated after recovery, including those over 65 years of age, a high risk group. In brief, reinfections were more than four times more likely in those who remained unvaccinated afterwards:
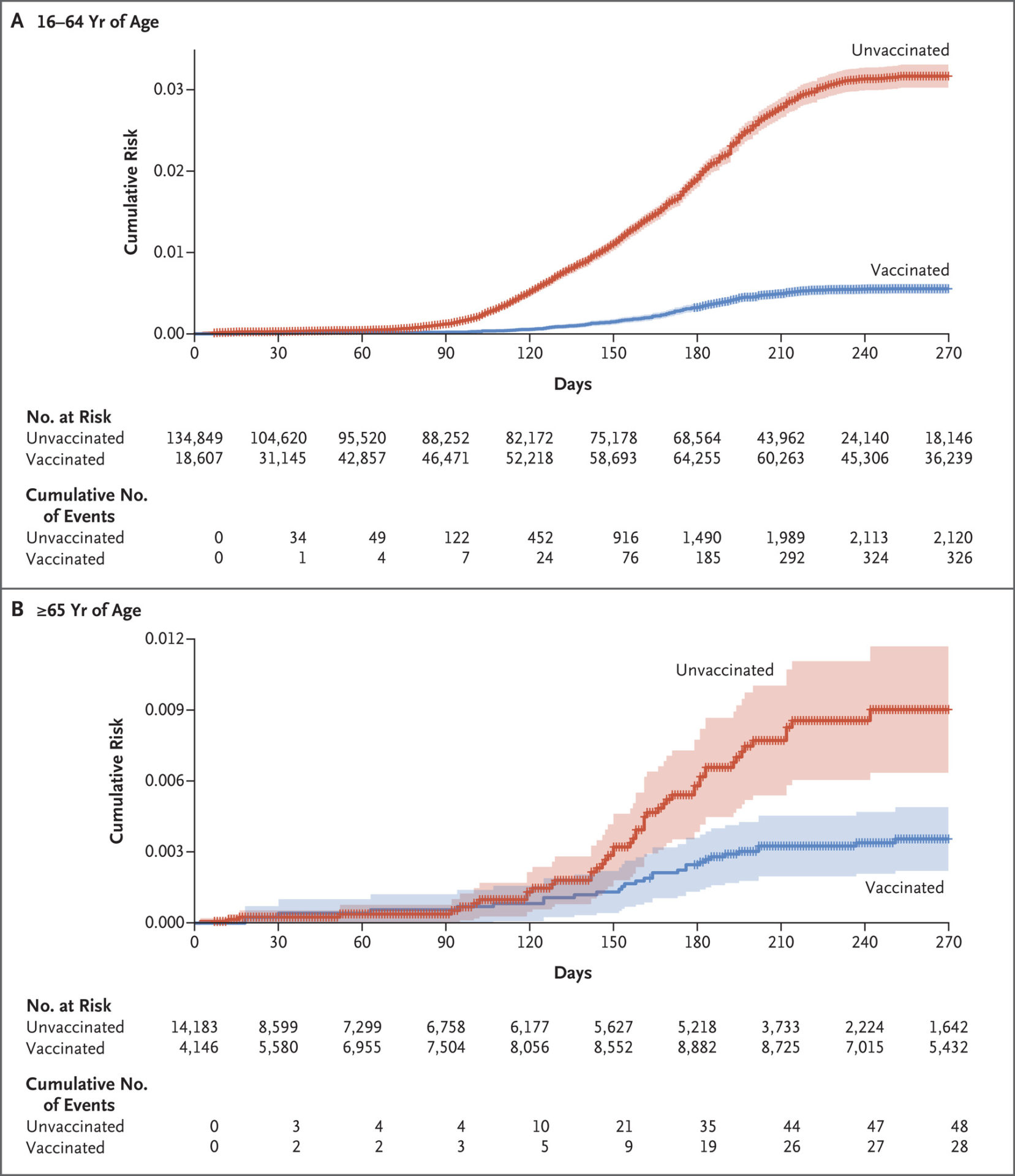
This study also found that there was no significant difference in vaccine effectiveness between those who received one dose or two doses after infection, in line with other studies suggesting that one dose of vaccine is sufficient in people preventing reinfection in people who recovered from COVID-19.
There are also laboratory studies that support the concept of hybrid immunity. Steve Novella wrote about one of them last month; so I won’t retread the same ground, other than to say that human immune sera following breakthrough infection and vaccination following natural infection (which contains the antibodies that neutralize the virus), broadly neutralize SARS-CoV-2 variants to a similar degree, implying that the order (infection, then vaccination, versus breakthrough infection after vaccination) doesn’t matter as much as the hybrid nature of the immunity and that the robust hybrid response was not diminished with age.
More recently, a recent study out of OHSU suggests that breakthrough infections work much the same way, finding substantial boosting of humoral (antibody-mediated) immunity after breakthrough infections after vaccination with the Pfizer/BioNTech vaccine, including against the Delta variant. A preprint from a different group suggests that the same occurs for Omicron after breakthrough infection. The limitations of these studies are that the numbers are small (52 in the first study, only 23 participants in the second, of which only 10 were breakthrough cases), but the studies did measure virus neutralization by immune serum from participants rather than just antibody titers. It won’t surprise me if larger studies confirm these observations about hybrid immunity, but I’ll wait until, at least, the second paper is published in a peer-reviewed journal.
Why does hybrid immunity appear to be more potent against SARS-CoV-2 and possibly longer lasting? According to one of the investigators of the SIREN study:
According to Crotty, hybrid immunity allows the body to create more diverse antibodies to neutralize a wider variety of variants. This also happens with full vaccination and a booster, but it happens much faster with infection followed by vaccination.
“Hybrid immunity has got a whole bunch of additional bonuses to it. One, that these studies are showing quite presently, is durability. Durability is quite robust,” Crotty said.
This makes intuitive sense, of course, although I always hasten to add that what is “intuitive” in science does not mean that it will turn out to be true. I will, however, point out that I really do not like one narrative that is coming from these studies, particularly the study that found enhanced immunity to other variants after breakthrough Omicron infection, that the Omicron variant could be “Mother Nature’s way of vaccinating the masses and curbing the pandemic, even going so far as to speculate that “omicron mimics these live attenuated vaccines because it causes milder infection and trains the body to trigger a strong immune response against the delta variant”. My response: Define “milder.”
And the beat goes on…
I started by asking whether “natural immunity” (a.k.a. postinfection immunity) was “better” than vaccine-induced immunity, which, it turns out, is the wrong question. Neither are “better”, but there are differences. Think of it this way. Given the risk of death and complications such as long COVID-19 and increasingly recognized cardiovascular complications from even mild disease, it is better not to get COVID-19. Thus, vaccination is preferable because it confers immunity without those potential risks and complications. However, contrary the narrative promoted by advocates of “natural herd immunity”, there’s nothing magical about “natural immunity”. It might or might not be more robust. It probably lasts longer, but, contrary to the magical properties ascribed to it those touting a “natural herd immunity” narrative, it is definitely not anywhere near lifelong, particularly against new variants, which means that “natural herd immunity” is almost certainly not achievable, although herd immunity might be achievable through a combination of vaccines and post-infection immunity. Moreover, if you have been unable to avoid getting COVID-19 and are fortunate enough to have recovered, it’s best to augment your “natural immunity” with vaccination because emerging evidence strongly suggests that hybrid immunity is the most robust immunity of all and helps protect more against new variants as well.
Contrary to the narrative being promoted by those who oppose vaccine mandates and advocate a “natural herd immunity approach”, no one in public health—and I mean no one—”denies natural immunity”. That part of the “natural immunity” narrative is one that I find profoundly insulting to physicians, scientists, public health officials, and vaccine advocates. It’s a massive straw man, which is why I’m going to quote this here:
Indeed, I would counter that the absolutists are the ones who tout post-infection “natural immunity” and “natural herd immunity” as being magically superior to vaccine-induced immunity to the point that it is the preferred way out of the pandemic, don’t recognize (or do their best to downplay) hybrid immunity, and minimize the harm and deaths that COVID-19 has caused—and continues to cause. In reality, scientists see nuance that the ideologues behind efforts of the GBD do not as they falsely portray their preferred solution and their contortions of science to justify it as “nuance” versus “vaccine absolutism”. They struggle to synthesize the flood of data—more often than we’d like, conflicting—into a science-based set of interventions that will minimize suffering and the loss of life and yet still be achievable without inflicting too much other harms. If that involves treating a prior COVID-19 infection like one course of vaccination (which might well be reasonable), so be it; contrary to how we are portrayed we are not dogmatically opposed to that. We merely want good evidence that this is a sound strategy in terms of minimizing the harm of the pandemic. In contrast, GBD proponents start from the idea that “lockdowns” do more damage than COVID-19 and, along with mask and vaccine mandates, are unacceptable assaults on individual freedom and then use motivated reasoning to find evidence to support their desired conclusion. Indeed, ask yourself why the same “anti-lockdowners” and antimaskers have aligned themselves with the antivaccine movement, given that no more powerful tool than the vaccines exists to implement an actual policy of “focused protection”.
As I’ve always said, we call it science-based medicine because medicine (and its related specialty public health) can never be purely science. Science can provide the parameters of what we can do by giving us interventions to combat the pandemic and telling us what the risk-benefit ratio of those interventions are, but in the end value judgments over the trade-offs involved are based on a given society’s values. Those behind the GBD have made it very clear what their values prioritize, and it’s definitely not the minimization of suffering and death. Unfortunately, they have also wielded outsized influence compared to their numbers, particularly among actual public health scientists.

